Learn more at AgingWellMetroDC.com
Living with Heart Failure
People with heart failure have good days and bad days. Sometimes a bad day requires a rush to the hospital. The goal is to reduce the triggers that tend to create a bad day. Here are some tips.
Avoiding crises with heart failure
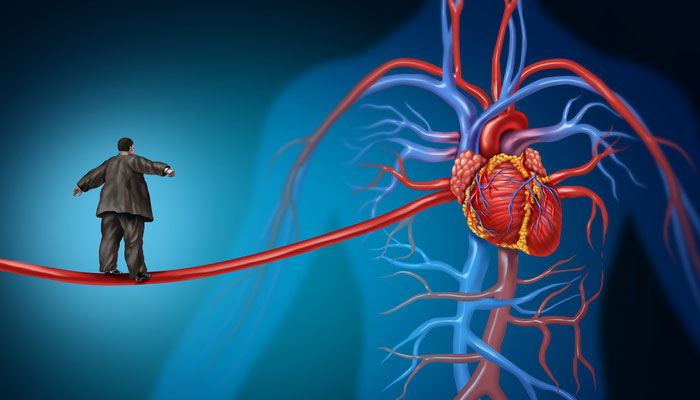
If your loved one has been diagnosed with heart failure (HF), it means there is a fluid buildup making it harder to pump blood.
The circulation backs up in the heart. Even the kidneys are affected, causing water gain in the legs, feet, and abdomen. This swelling, called “edema,” adds pounds to the body’s weight. And any extra weight, in turn, means extra work for an already-stressed heart. When this cycle of fluid buildup goes unchecked, it also can make breathing harder and trigger a medical emergency. Perhaps even the need for hospitalization.
To avoid a crisis, check for these signs EVERY DAY:
- Sudden weight gain or loss. Have your loved one weigh first thing in the morning, right after urinating and before drinking or eating.
- Swelling in the abdomen. Check how clothing fits; look especially for tightness, tenderness, or bloating at the waist.
- Fatigue, shortness of breath even when resting. Note any complaints of weakness, dizziness, or a desire to reduce activity.
If you observe any one of these symptoms, contact your loved one’s doctor immediately for guidance. The doctor may recommend changes in the day’s diet or fluid intake. Or changes in medication. The American Heart Association has a free HF Path app to help track symptoms. Create an account at their website or download it for smartphones at iTunes or Google Play.
Check with the doctor about other self-care activities that may help reduce the likelihood of an emergency. For example:
- Sitting or lying down with legs elevated to help blood flow to the heart.
- Wearing specialized stockings to help minimize fluid buildup in the legs.
- Lightly stroking or massaging legs, or doing simple exercises, to get the fluid moving.
- Reducing salt and fluid intake.
Addressing Fatigue

People with HF often tire easily, especially if they exert themselves. A heart swollen with fluids cannot beat efficiently. The body’s cells then become hungry for oxygen. If your loved one has HF, you witness this in his or her fatigue, shortness of breath, and frequent naps.
Even with HF, however, your relative needs to be physically active. Physical activity helps the heart muscle gain strength. It improves circulation. It helps with weight control, and, oddly, with reducing fatigue. Exercise also helps with depression, which is common in HF.
Pacing is the key. Talk with the doctor about optimal forms of physical activity. Initially, walking, swimming, or biking may be recommended. As HF progresses, simple tasks, such as taking a shower or cooking a meal, may qualify as exercise. Ask the doctor for a prescription to work with a cardiac rehab team to create an activity plan tailored to your loved one’s needs.
Conserving energy. Think of personal energy as a tank of gas. With HF, your relative has a small tank and needs to be “fuel efficient.” Conserving energy when doing chores leaves more “in the tank” for doing things that bring joy and meaning.
- Alternate periods of activity with periods of rest. Divide large chores into smaller tasks throughout the day or across the week.
- Avoid rushing. It wastes energy.
- Work smarter. Minimize trips up or down stairs. Cook large quantities of food and freeze for heating later. Instead of towel drying, slip on a terry cloth bathrobe after bathing.
- Get help for mundane tasks. Have groceries and prescriptions delivered.
- Create workstations that permit cooking, grooming, dressing, and bathing while seated.
- Use a cart or walker with a basket for carrying things from place to place.
- Avoid bending or reaching. Use extenders.
Reducing Salt
This is admittedly not a popular suggestion. Salt (sodium) makes food tastier. But salt is a key factor in reducing the swelling that causes breathing, fatigue, and sleep issues for those with HF. There are three key strategies for reducing salt:
Remove the main sources of salt. (These two steps reduce salt intake by 30%!)
- Take the saltshaker off the table.
- Remove the salt supply from the kitchen (including soy sauce).
Add flavor with herbs and spices. Experiment.
- At the table: no-salt dried herb blends, lemon juice, balsamic vinegar, freshly ground pepper, toasted sesame oil.
- In cooking: fresh or dried savory herbs (basil, thyme, sage), exotic spices (curry, ginger, chipotle pepper), citrus juice, and grated citrus rind.
Do not provide a commercial “salt substitute” without the doctor’s permission.
Reduce or eliminate commercially prepared foods. An entire day’s “salt budget” can be blown in a single serving of prepared dinners, luncheon meats, quick breads/cereals, and common condiments and marinades. Instead:
- Read labels and buy only low-sodium foods.
- Rinse canned vegetables or tuna to wash away extra salt.
- Serve salad dressings or sauces on the side. People use far less if they dip their food in rather than pour the sauce or dressing over.
- Make mixes. Make your own mixes for pancakes, cornbread, and muffins with low-sodium baking powder.
- Be cautious about over-the-counter medicines. Heartburn and headache drugs often contain sodium.
Contact us at 301-593-5285
