Our Monthly Newsletter
Helpful tips for family caregivers
August/September 2017
Driving, Medicare and food. These rank high on a list of caregiving support tasks. This month we have some insights to help you in these key areas. For instance, if a new car is in your future, check out our tips for features that will make your auto caregiver-friendly. Then there’s Medicare. Interesting changes in payments to medical providers hold promise to bring improvements on several fronts. Heartburn anyone? This is the most frequent digestive problem in older adults. Learn about foods that make heartburn worse and need to be avoided.
The caregiver-friendly car
 If a new car is in your future—even just a new-to-you car—look for features that support your role as a family caregiver.
If a new car is in your future—even just a new-to-you car—look for features that support your role as a family caregiver.
For instance, extra room for carrying things can make your job a lot easier!
More important, look for features that will protect your back as you help your loved one in and out of the car. Back injuries are painful and costly. They are the number one physical problem among family caregivers.
Consider these features before you buy a car:
- Height of the car. Avoid low-slung cars with bucket seats, or elevated trucks and SUVs. Choose instead a mid-height sedan, minivan, or crossover vehicle.
- Practice the transfer. Go through the motions your loved one would use to get into and out of the car. Is there something to hang onto in both directions (handle over the door, handle of the door, seat back, etc).
- Electric seats are a plus. You may have to adjust seat position each time your relative gets in the car. Save your back! Check out the maneuverability of the backseat, too. If your loved one has moderate dementia, it is best for him or her to ride in the rear.
- Keyless doors and locks. Remote, pushbutton opening leaves your hands free to help your relative. It is also useful if you are carrying equipment or supplies.
- Room for a walker or wheelchair. If the person you care for already has one of these mobility aids, take it with you when you shop for a car. Can you fit the walker in behind the front seat? Or will it have to take up space in the trunk? Can you easily and safely lift a wheelchair in and out of the cargo space?
- Electric windows and locks. People with dementia have been known to open the door while in a moving car. Look for the “child safety” feature that allows the driver to control the windows and doors.
- Heated and cooled seats. Older adults often have trouble regulating their temperature. If possible, buy a car that provides heating or cooling individually for each seat.
Medicare's Triple Aim
 There is a lot of talk about health care funding. What you may not know is that Medicare has been implementing many new strategies on the provider—doctor and hospital—side. They are designed to reduce costs while also improving patient care and satisfaction. Termed the “Triple Aim,” these service changes are Medicare’s way of promoting more patient-centered care.
There is a lot of talk about health care funding. What you may not know is that Medicare has been implementing many new strategies on the provider—doctor and hospital—side. They are designed to reduce costs while also improving patient care and satisfaction. Termed the “Triple Aim,” these service changes are Medicare’s way of promoting more patient-centered care.
You may already be noticing more
- educational support. If your loved one has a chronic condition, new services or classes may be available to help. Many of the most effective treatments are not medicines but lifestyle changes. Medicare is willing to pay for services such as cardiac rehab programs and diabetes education.
- willingness to meet by phone. New regulations allow doctors to bill Medicare for telephone visits. This is efficient for the doctor. And it saves you the hassle of driving to the office and sitting in a waiting room.
- shared decision making. Don’t be surprised if your loved one’s provider asks, “What would you hope to be able to do if this treatment is successful?” Your relative might say, for example, “Work in my garden again,” or “Attend my book club meetings.” Providers will walk through the pros and cons of treatment options based on each patient’s individualized goals. This is key to patient-centered care.
- attention to family caregivers. There is new recognition that family members are valued members of the health care team. Providers are starting to acknowledge that family caregivers need support, instruction, and care themselves so they don’t burn out.
- ratings focus. From nursing homes to hospitals, Medicare is asking patients to give feedback. The feedback is public. In many cases, poor satisfaction scores affect how much providers get paid.
If you have not been offered these services, ask! You and your loved one have the right to high-quality care. Medicare is taking the Triple Aim very seriously.
Return to topIs heartburn a problem?
 If you’ve ever had heartburn, you know how painful it can be. Sometimes the symptoms mimic those of a heart attack!
If you’ve ever had heartburn, you know how painful it can be. Sometimes the symptoms mimic those of a heart attack!
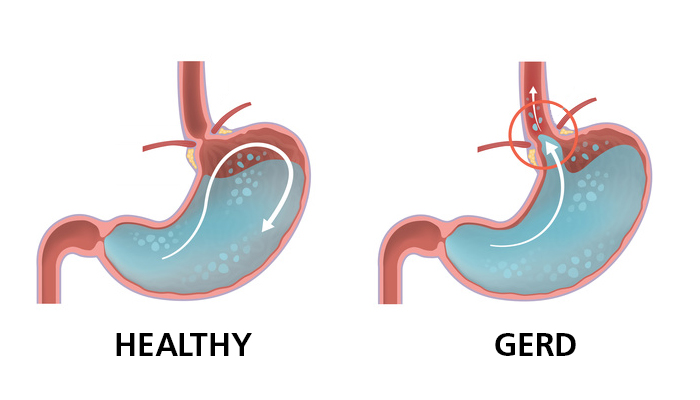
The underlying cause involves acid from the stomach sloshing up onto the sensitive lining of the esophagus, the tube that connects the throat to the stomach.
This condition is called GERD: gastroesophageal reflux disease. The primary symptom is a burning sensation in the center of the chest. Other symptoms include
- belching after a meal and bringing up a bit of food or sour, burning liquid;
- trouble swallowing;
- feeling like there’s a lump in the throat;
- hoarse voice;
- dry cough.
 Get a diagnosis. If you suspect your relative has GERD, get a formal diagnosis from the doctor—just to be sure it’s not something more serious.
Get a diagnosis. If you suspect your relative has GERD, get a formal diagnosis from the doctor—just to be sure it’s not something more serious.
GERD should be treated. Besides discomfort, more critical problems can develop. GERD is extremely common in older adults. They typically report fewer symptoms but also tend to have more complications.
Seek medical help immediately if you or the person you care for experiences severe chest pain. While it may be GERD, it truly could be a heart attack. Better to be safe.
Lifestyle changes. If GERD has been confirmed, lifestyle changes are the first line of defense.
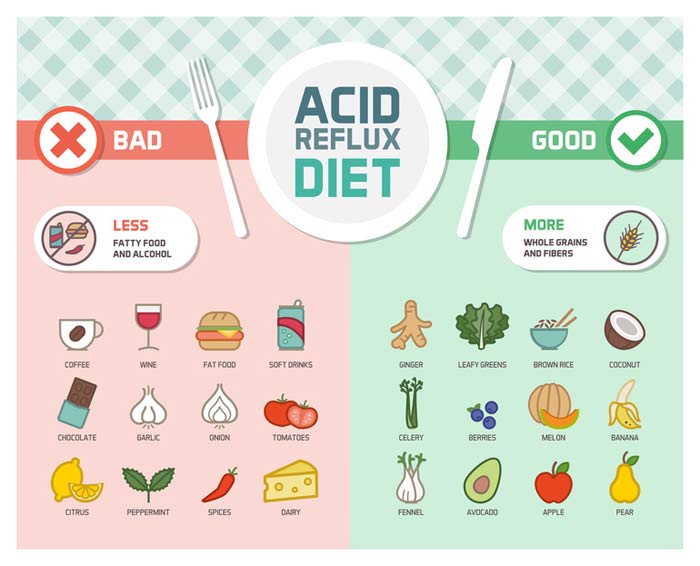
- Eat differently. Avoid high-fat foods, alcohol, tomato sauce, chocolate, garlic, onion, mint, and caffeine (the fun stuff, darn it!).
- Lose weight. Extra pounds around the belly push the stomach upward.
- Wear loose clothing. A tight waistband also puts pressure on the stomach.
- Eat smaller meals.
- Elevate the head of the bed. Use bricks under the legs at the head end, or a wedge. Pillows don’t solve the problem.
- Wait 3 hours after eating before lying down.
Other treatments. If over-the-counter medicines don’t provide relief, the doctor may recommend a prescription. In unusual cases, surgery is required.
Return to top